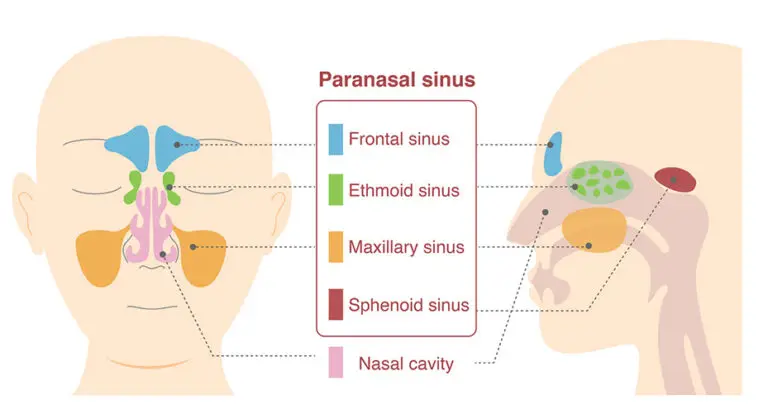
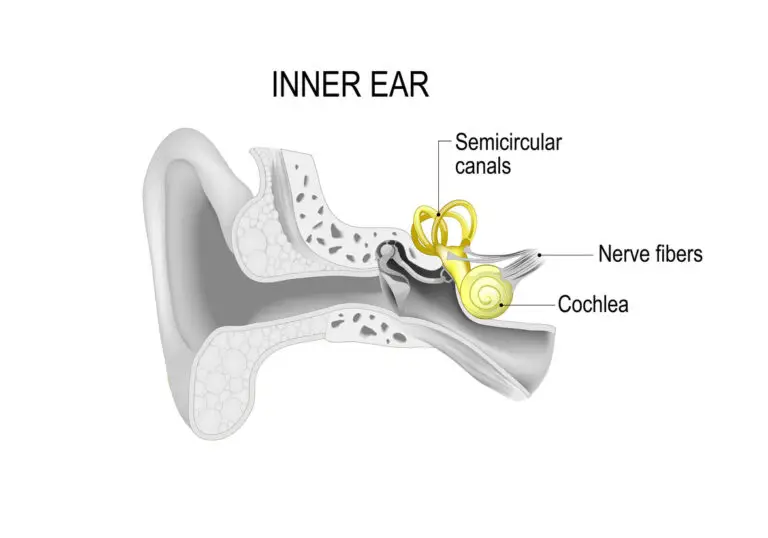
Peripheral vestibular disorders, or PVDs, are conditions that affect the inner ear. The inner ear plays an important role in helping a person keep their balance and understand their physical position as they move.
The primary symptom of a Peripheral Vestibular Disorder (PVD) is dizziness, often described as a sensation of the room spinning, known medically as vertigo. This sensation frequently prompts individuals to seek medical help. 1
Several medical conditions can lead to PVDs, with Benign Paroxysmal Positional Vertigo (BPPV) and Meniere’s disease being the most prevalent. BPPV falls under the PVD rating criteria for VA disability, while Meniere’s disease has its own diagnostic code, 6205, and a distinct rating schedule.
PVDs may arise from traumatic brain injuries, motor vehicle accidents, viral and ear infections, Eustachian tube dysfunction, sinus diseases, and aging. 2,3
Veterans experiencing PVD symptoms should document them in a Statement in Support of Claim.
This post offers insights into PVDs concerning VA disability.
History of Peripheral Vestibular Disorder
During a Compensation and Pension (C&P) exam, the veteran’s PVD history is recorded using the Ear Conditions Disability Benefits Questionnaire (DBQ). Section II provides a summary, while Section III delves into symptoms relevant to the rating schedule.
The DBQ history for PVD inquires about:
- Vertigo: Frequency and duration of dizziness
- Staggering: Frequency and duration of difficulty walking as if going to fall
- Tinnitus: Frequency and duration of ringing in the ear
- Hearing Loss: If present and associated with PVD, the C&P examiner will document it and may refer for audiological testing.
The frequency and duration of symptoms associated with PVD does not affect the disability rating under code 6204 but is significant for Meniere’s disease under code 6205.
Physical Examination for Peripheral Vestibular Disorder
C&P examiners may carry out a physical exam during VA disability evaluations. Although the inner ear is not visible, the examiner inspects the outer ear and uses an otoscope for the ear canal, potentially viewing the tympanic membrane. Examiners might assess the veteran’s movement and administer tests like the Romberg Test, Dix Hallpike test, or limb coordination test, which require no special equipment.
Testing for Peripheral Vestibular Disorder
Imaging studies are often part of the clinical assessment but not routinely included in C&P exams. The CFR mandates objective evidence of PVD for a compensable evaluation, urging veterans to seek clinical evaluation and testing independently.
Other tests, such as electronystagmography (ENG), are not conducted in primary care and require a specialist.
If unavailable, testing is not typically ordered during C&P exams.
Treatment for Peripheral Vestibular Disorder
PVD treatment may include maneuvers to restore inner ear balance, performed by specialists, and prescription medications for symptom relief.
Ratings for Peripheral Vestibular Disorders
Veterans seeking disability ratings for PVD can refer to code 6204 in the CFR.
The CFR reports that “objective findings” supporting the diagnosis of PVD are require before a compensable evaluation can be assigned. Additionally, if the veteran has hearing impairment or tinnitus, it shall be separately rated.
The rating schedule evaluates PVD as follows:
- 10% Rating
- Occasional dizziness
- 30% Rating
- Dizziness
- Occasional staggering
Further Learning
For further information, tune into the Valor 4 Vet and Exposed Vet Radio Show from October 3, 2024.
The Ear Conditions DBQ can be found here.
The M21-1 on Peripheral Vestibular and Other Ear Disorders is also available for additional reading.
References
1. Venosa, Alessandra Ramos and Roseli Saraiva Moreira Bittar, 2007. “Vestibular rehabilitation exercises in acute vertigo”, The Laryngoscope(8), 117:1482-1487. https://doi.org/10.1097/mlg.0b013e318068b54f
2. Hwang, Sang Yun, Saskia E. Kok, and Judie Walton, 2016. “Balloon dilation for eustachian tube dysfunction: systematic review”, The Journal of Laryngology &Amp; Otology(S4), 130:S2-S6. https://doi.org/10.1017/s0022215116008252
3. Pastakia, Khushnum and Saravana Kumar, 2011. “Acute whiplash associated disorders (wad)”, Open Access Emergency Medicine:29. https://doi.org/10.2147/oaem.s17853